The complexity of modern healthcare is growing exponentially, and clinicians are expected to process vast streams of data, ab results, imaging, genomics, medications, clinical notes, all while maintaining patient safety, efficiency, and compliance.
This is where clinical decision support becomes indispensable.
Clinical decision support systems (CDSS), also known as clinical decision support tools or clinical decision support software, help clinicians make evidence-based decisions at the point of care.
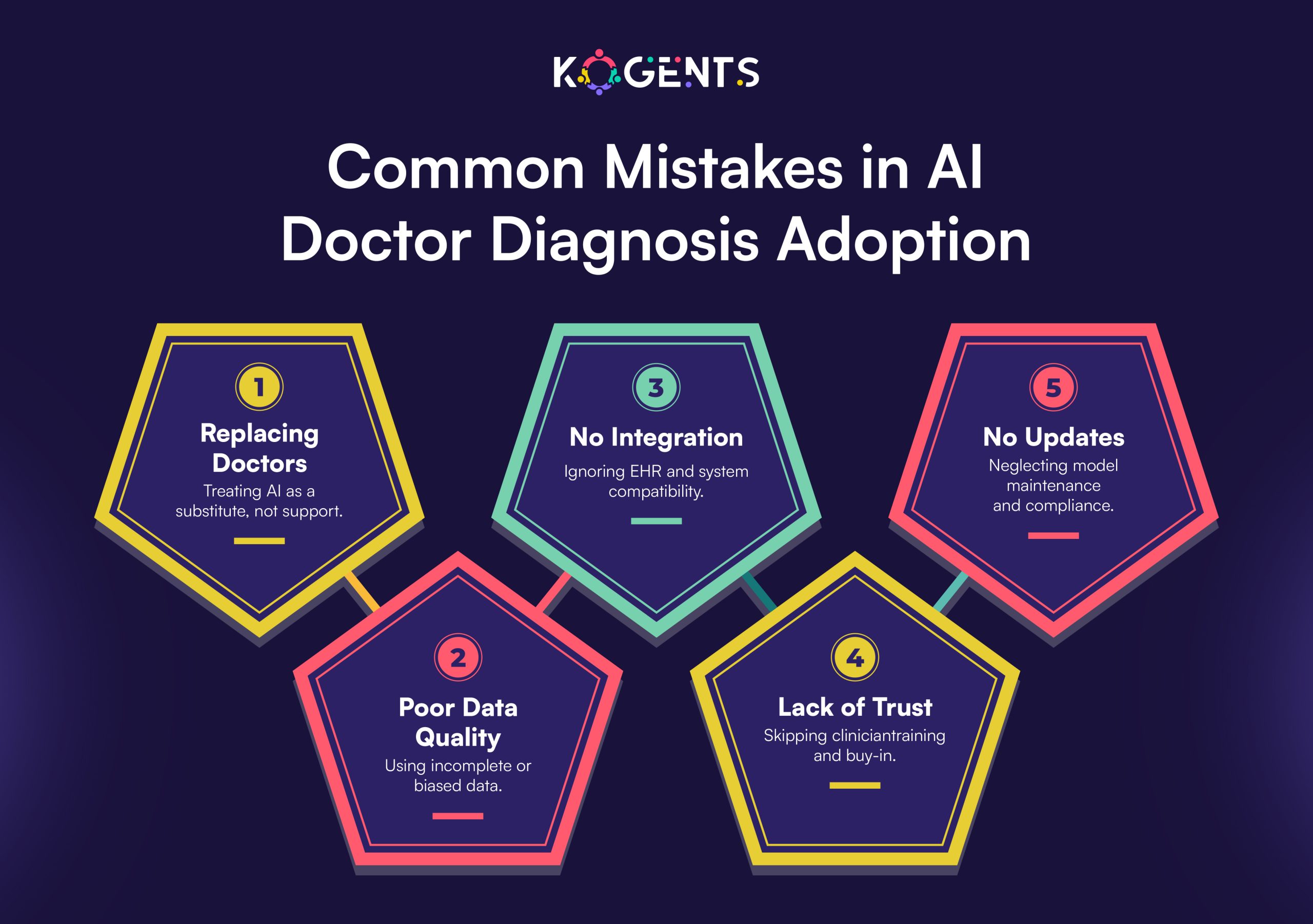
Yet as hospitals scale, integrating these tools securely across diverse electronic health record (EHR) systems becomes a formidable challenge.
Enter AI agents, intelligent, autonomous systems capable of interpreting clinical data, reasoning contextually, and interacting seamlessly with EHRs.
When designed responsibly, AI-based clinical decision support systems can unify fragmented data, reduce alert fatigue, and enhance outcomes, all while maintaining compliance and data security.
This article explores how AI agents are enabling scalable, secure, and interoperable clinical decision support platforms across enterprise healthcare environments.
Key Takeaways
- How AI-driven clinical decision support enhances diagnosis and care quality.
- The importance of scalable, secure integration across enterprise EHR systems.
- How interoperability standards enable seamless data exchange in healthcare.
- The role of privacy-preserving AI and compliance in modern CDS platforms.
- Why adaptive, intelligent systems are redefining clinical workflows and outcomes.
What Is Clinical Decision Support (CDS)?
It is a foundational element of health informatics that delivers patient-specific insights, alerts, and recommendations to improve clinical decisions.
A clinical decision support system (CDSS) typically integrates data from multiple sources, EHRs, lab systems, and knowledge bases, to present relevant, actionable information to clinicians.
These tools can be rules-based, relying on pre-set algorithms (“If patient’s potassium < 3.0 → suggest supplementation”), or predictive decision support systems powered by machine learning that adapt to new evidence over time.
Moreover, modern clinical decision support platforms increasingly employ AI, natural language processing (NLP), and predictive modeling to analyze both structured (lab data, vitals) and unstructured data (physician notes, discharge summaries).
This enables context-aware, evidence-based decision support tailored to individual patient needs.
Key benefits:
- Reduces diagnostic errors and adverse events
- Enhances adherence to clinical guidelines
- Improves workflow efficiency and patient outcomes
- Strengthens clinical quality measures and compliance tracking
The Enterprise EHR Challenge
Scaling clinical decision support software across large healthcare organizations introduces both technical and regulatory challenges.
Data Silos and Interoperability
- Hospitals often operate on different EHR vendors (Epic, Cerner, Allscripts), making data exchange difficult.
- Further, even with standards like HL7 and FHIR, true interoperability remains elusive due to varied implementations, inconsistent data schemas, and limited support for real-time communication.
Security and Compliance Risks
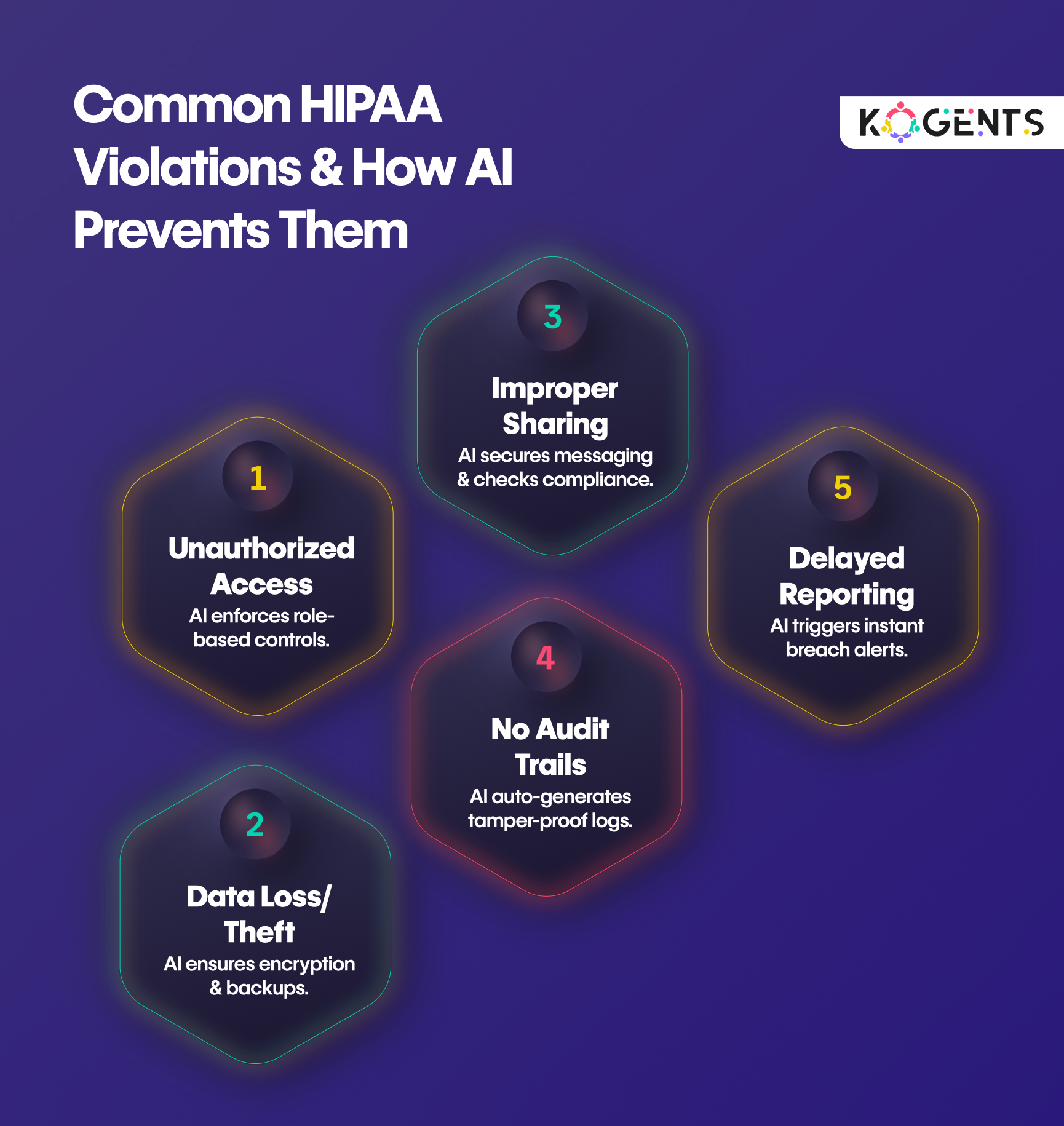
- Protected health information (PHI) must comply with HIPAA, GDPR, and HITECH.
- Transmitting patient data between systems introduces vulnerabilities unless encryption, access control, and audit logs are meticulously enforced.
Alert Fatigue and Workflow Integration
- When poorly designed, clinical decision support tools overwhelm clinicians with irrelevant alerts, leading to alert fatigue and missed warnings.
- This challenge underscores the need for contextual awareness and usability-driven design.
Scalability and Governance
- Each hospital or region may have unique clinical workflows and protocols.
- Scaling a clinical decision support platform requires modular, adaptable infrastructure, one that can update rules, guidelines, and algorithms across thousands of users without disrupting care.

How AI Agents Transform Clinical Decision Support?
The emergence of AI agents for healthcare automation represents a paradigm shift in clinical decision support systems (CDSS).
Unlike static rule engines, AI-driven CDS continuously learns, reasons, and collaborates with clinicians in real time.
Key Capabilities of AI Agents in CDS:
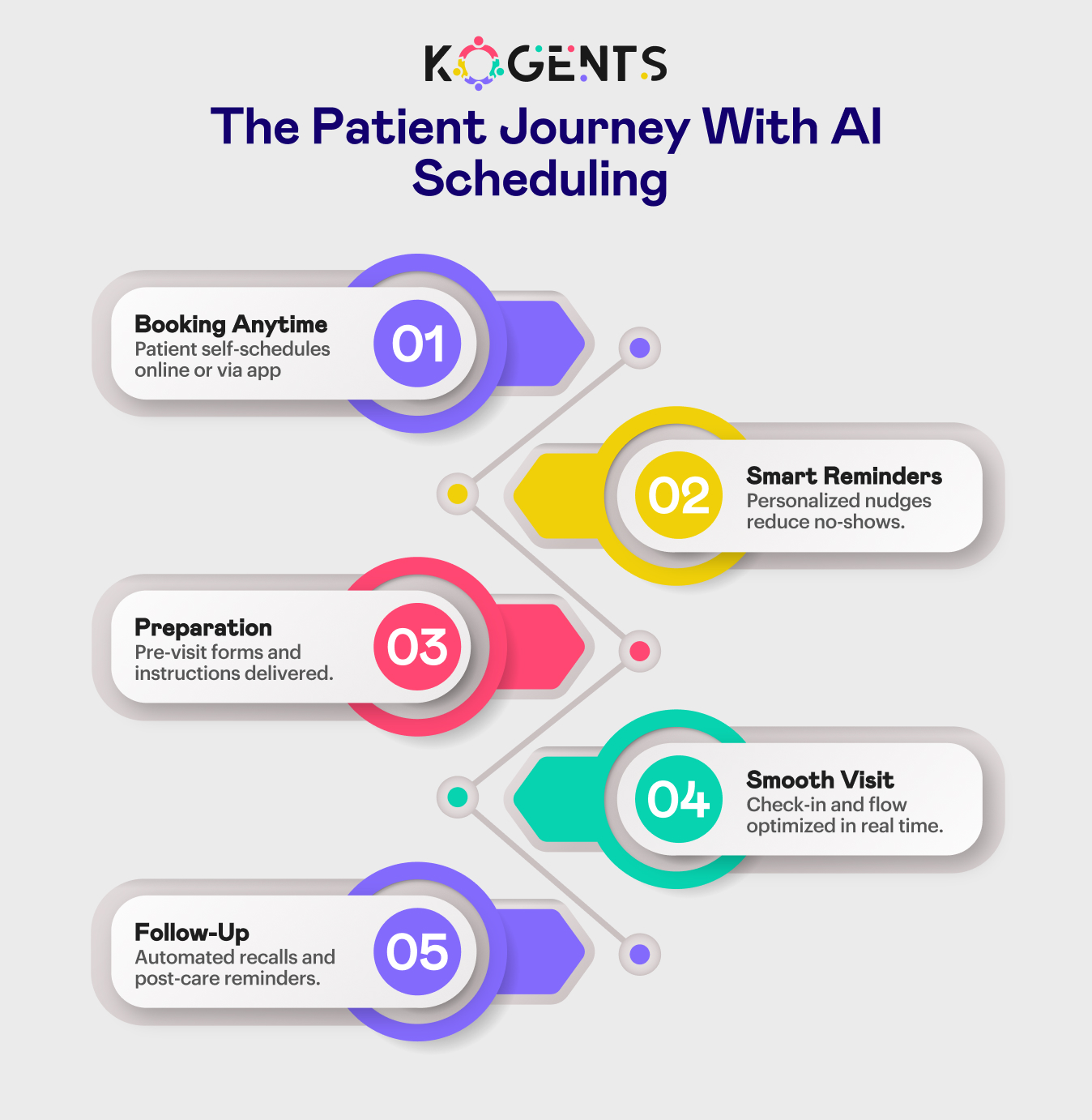
- Continuous Learning: AI agents ingest real-world data, outcomes, and feedback to refine decision logic. This creates a learning health system that improves with every AI patient scheduling and interaction.
- Predictive and Contextual Analysis: Using machine learning and natural language processing, AI agents analyze structured and unstructured data to predict events like sepsis, adverse drug reactions, or readmission risks.
- Explainable AI (XAI): Transparency is vital in healthcare, and techniques such as SHAP and LIME allow clinicians to understand why an AI agent recommends a certain action, maintaining trust and accountability.
- Interoperability and Integration: Through FHIR-based APIs, AI agents integrate seamlessly with diverse EHRs, enabling interoperable clinical decision support without custom coding for each vendor.
- Workflow Intelligence: AI agents detect contextual signals, clinician specialty, patient acuity, time of day, and tailor alerts to minimize alert fatigue while improving clinical workflow efficiency.

Case Study 1: Sepsis Prediction at a Major U.S. Health Network
A multi-hospital system integrated an AI-based clinical decision support platform powered by agents that monitored EHR streams for sepsis risk indicators.
- Result: Early warning alerts 4 hours before traditional systems.
- Impact: 24% reduction in sepsis mortality, 31% fewer ICU transfers.
- Compliance: Fully aligned with the FDA’s SaMD and HIPAA standards using secure federated learning.
Note: This demonstrates how AI agents for health care automation make predictive decisions to support scalable, secure, and life-saving.
Scaling CDS Across Enterprise EHR Systems
To deliver value enterprise-wide, clinical decision support systems must scale without compromising performance, security, or accuracy.
Scalable Architecture
A modular design built on microservices enables hospitals to deploy CDS components independently, from rules-based engines to predictive AI modules.
Containerization (Docker, Kubernetes) supports load balancing and fault tolerance across multiple facilities.
Federated Learning for Privacy-Preserving Scale
Traditional model training centralizes sensitive patient data.
Besides, in contrast, federated learning allows local models to learn independently while sharing only encrypted parameters.
This ensures compliance with HIPAA, GDPR, and emerging FDA AI/ML guidelines.
Standardized Data Interoperability
Adherence to FHIR, SNOMED CT, LOINC, and ICD-10 standards ensures that AI agents interpret data consistently across institutions. This is a cornerstone not only for interoperable clinical decision support but also for reliable AI doctor diagnosis frameworks.
| Scaling Strategy | Description | Key Benefits |
| FHIR-Based APIs | Unified integration with EHR systems using HL7/FHIR standards | Reduces integration costs and time |
| Federated Learning | Decentralized model training without sharing raw patient data | Ensures HIPAA/GDPR compliance |
| Microservices Architecture | Modular, containerized services | Enables scalability and fault tolerance |
| Edge AI Deployment | Local inference for real-time responsiveness | Improves latency and data control |
| Unified Governance Layer | Centralized model oversight and rule management | Ensures regulatory consistency |
Key Point: These strategies allow EHR-integrated decision support to function enterprise-wide, delivering consistent and evidence-based clinical decision making while safeguarding data.
Case Study 2: Predictive CDS Across a European Hospital Consortium
A consortium of five hospitals in the EU deployed an AI-driven clinical decision support engine to predict patient deterioration.
- Integrated with five distinct EHR systems via FHIR APIs.
- Achieved 99.8% data integrity through on-premise encryption.
- Resulted in a 17% reduction in hospital readmissions and faster ICU triage.
This case illustrates that scalability is not just about computing power; it’s about intelligent, compliant architecture.
Ensuring Security, Privacy, and Compliance At Your Assistance
Trust is non-negotiable in healthcare technology. Clinical decision support platforms must uphold the highest standards of security, transparency, and regulatory compliance.
Core Security Practices
- End-to-End Encryption for all data in motion and at rest.
- Role-Based Access Control (RBAC) to ensure only authorized users have access to PHI.
- Immutable Audit Trails to document every decision, data access, and algorithm update.
Privacy-Preserving AI
Using federated learning, differential privacy, and data anonymization, organizations can maintain algorithmic performance without sharing raw patient data.
Regulatory Alignment
AI-driven CDS solutions must comply with:
- HIPAA (U.S.)
- GDPR (EU)
- FDA SaMD Guidance
- ONC Health IT Certification
Note: These frameworks ensure algorithmic transparency, explainability, and patient safety.
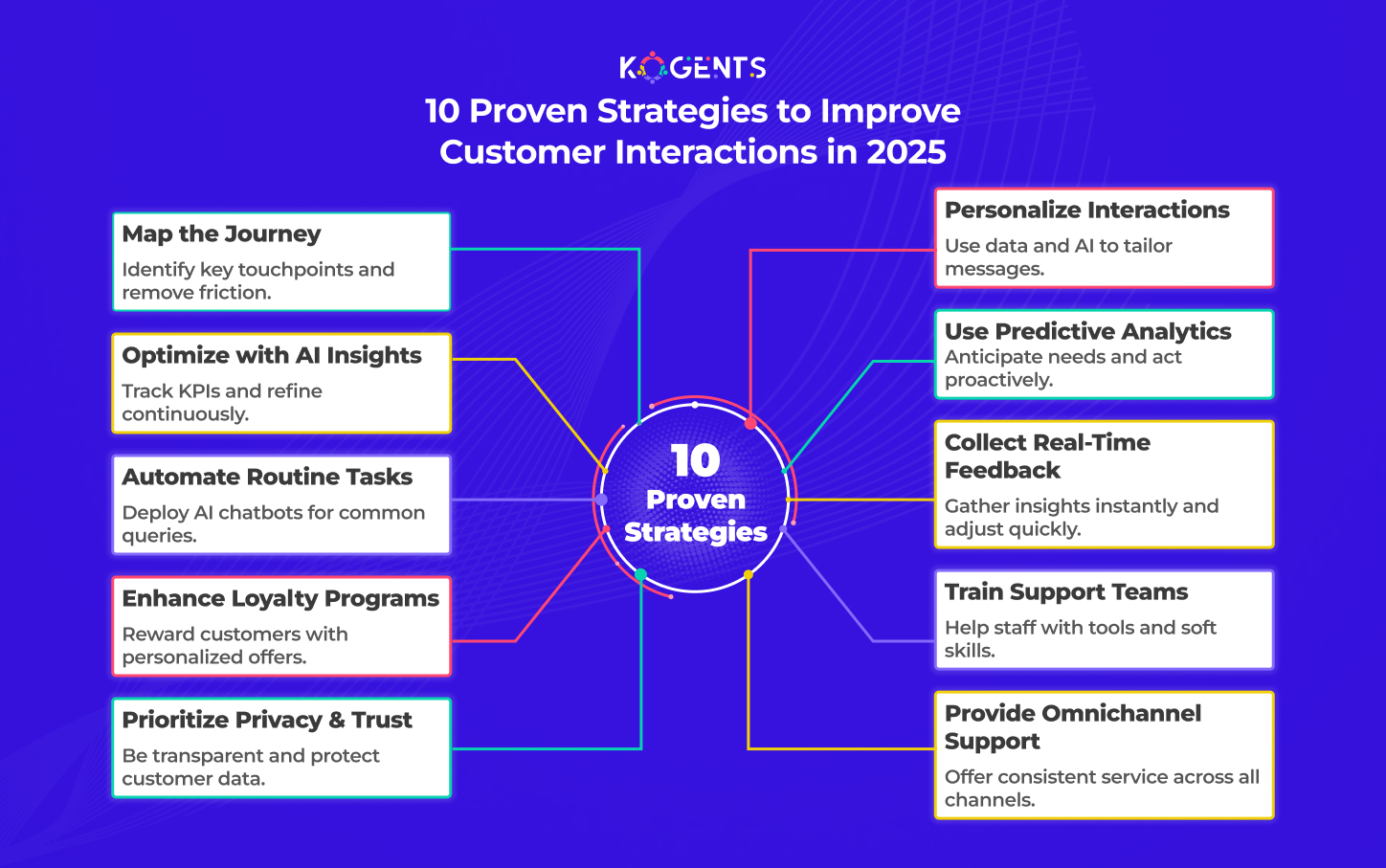
Implementation Strategies for Healthcare Enterprises
To succeed, healthcare organizations must approach CDS implementation as both a technical and cultural transformation.
1. Establish Governance
Define policies for algorithm validation, clinician oversight, and version control to meet medical liability standards.
2. Standardize Data Models
It’s feasible to adopt HL7 FHIR, CQL, and Arden Syntax for unified, interoperable frameworks.
3. Start Small, Scale Fast
Pilot point-of-care decision support for specific clinical pathways (e.g., antibiotic stewardship, radiology appropriateness) before full-scale rollout.
4. Integrate Clinician Feedback
Usability is critical, and that is why it must incorporate feedback loops for continuous improvement of alert thresholds, UX, and data presentation.
5. Choose Vendor-Neutral Platforms
Solutions like Kogents.ai provide modular AI agent orchestration that integrates with any EHR vendor, ensuring future-proof interoperability.
The Future of AI-Driven Clinical Decision Support
Healthcare is evolving toward a learning health system, one that continuously improves by analyzing outcomes and adapting decision logic.
Emerging Trends:
- Generative AI for Clinical Documentation: Automatically summarize visits, create structured notes, and suggest next steps aligned with guidelines.
- Collaborative AI Agents: Multiple agents working together, for example, one managing medications while another predicts complications.
- Predictive Population Health Management: Using AI-driven clinical decision support to identify at-risk groups early.
- Explainable and Ethical AI: Reinforcing algorithm transparency, fairness, and model drift monitoring.
Know the Highlight: Ultimately, the convergence of EHR-integrated decision support, AI orchestration, and secure interoperability will redefine clinical care delivery.
Transforming Healthcare Intelligence with Kogents.ai!
Clinical decision support systems have evolved from static alert engines into intelligent, adaptive platforms that drive safer, smarter care.
But the future belongs to AI-driven, interoperable, and secure clinical decision support, the kind enabled by autonomous AI agents.
By combining machine learning, federated architectures, and evidence-based decision logic, healthcare organizations can transform scattered data into a cohesive intelligence ecosystem.
These systems not only improve clinical decision-making but also foster a learning health system capable of continuous self-improvement.
But, the question is, are you ready to bring scalable, secure, and explainable AI into your clinical workflows?
If yes, then partner with Kogents.ai, the platform purpose-built for deploying AI agents that power interoperable clinical decision support systems, unify EHR data, and deliver enterprise-grade performance with regulatory confidence. Give us a call at +1 (267) 248-9454 or drop an email at info@kogents.ai.
FAQs
What is clinical decision support (CDS)?
Clinical decision support provides clinicians with actionable, data-driven insights during care delivery. It combines clinical guidelines, EHR data, and predictive algorithms to enhance patient outcomes.
How does AI enhance clinical decision support systems (CDSS)?
AI introduces context awareness, predictive analytics, and continuous learning. This reduces false positives and alert fatigue, delivering more relevant recommendations.
What are the types of CDS tools we must be aware of?
- Rules-based decision support
- Predictive decision support (AI/ML)
- Guideline-driven decision support
- Workflow-integrated clinical decision support
What are the benefits of integrating CDS with EHRs?
EHR-integrated decision support ensures real-time access to patient context, improving efficiency, compliance, and care coordination.
What limits CDS scalability?
Barriers include data silos, lack of interoperability, and security constraints across EHR systems.
How does the FDA regulate AI-based CDS?
The U.S. FDA governs clinical decision support software as part of its Software as a Medical Device (SaMD) framework, requiring validation, transparency, and explainability.
How can healthcare systems secure CDS deployments?
By implementing encryption, federated learning, and audit trails, and maintaining compliance with HIPAA, GDPR, and HITECH.
What’s the difference between CDS and general decision support systems?
While general systems apply to business or logistics, clinical decision support systems rely on clinical knowledge bases, evidence-based medicine, and regulatory compliance.
How do AI agents collaborate with clinicians?
They act as intelligent co-pilots, providing real-time insights while clinicians retain final authority over patient care.
What’s the ROI of deploying enterprise CDS?
Hospitals report reduced adverse events, improved clinical quality metrics, and measurable financial ROI within 12–24 months.