Every year, healthcare providers lose millions of dollars to poor insurance verification processes, one of the most preventable yet persistent forms of revenue leakage in modern medical operations.
Much of this loss stems from outdated manual workflows: staff spending hours making payer calls, navigating confusing IVR menus, waiting on hold, manually documenting benefits, and often entering incorrect or incomplete information.
These inefficiencies lead to claim denials, delayed reimbursements, inaccurate patient estimates, and skyrocketing accounts receivable (A/R) days.
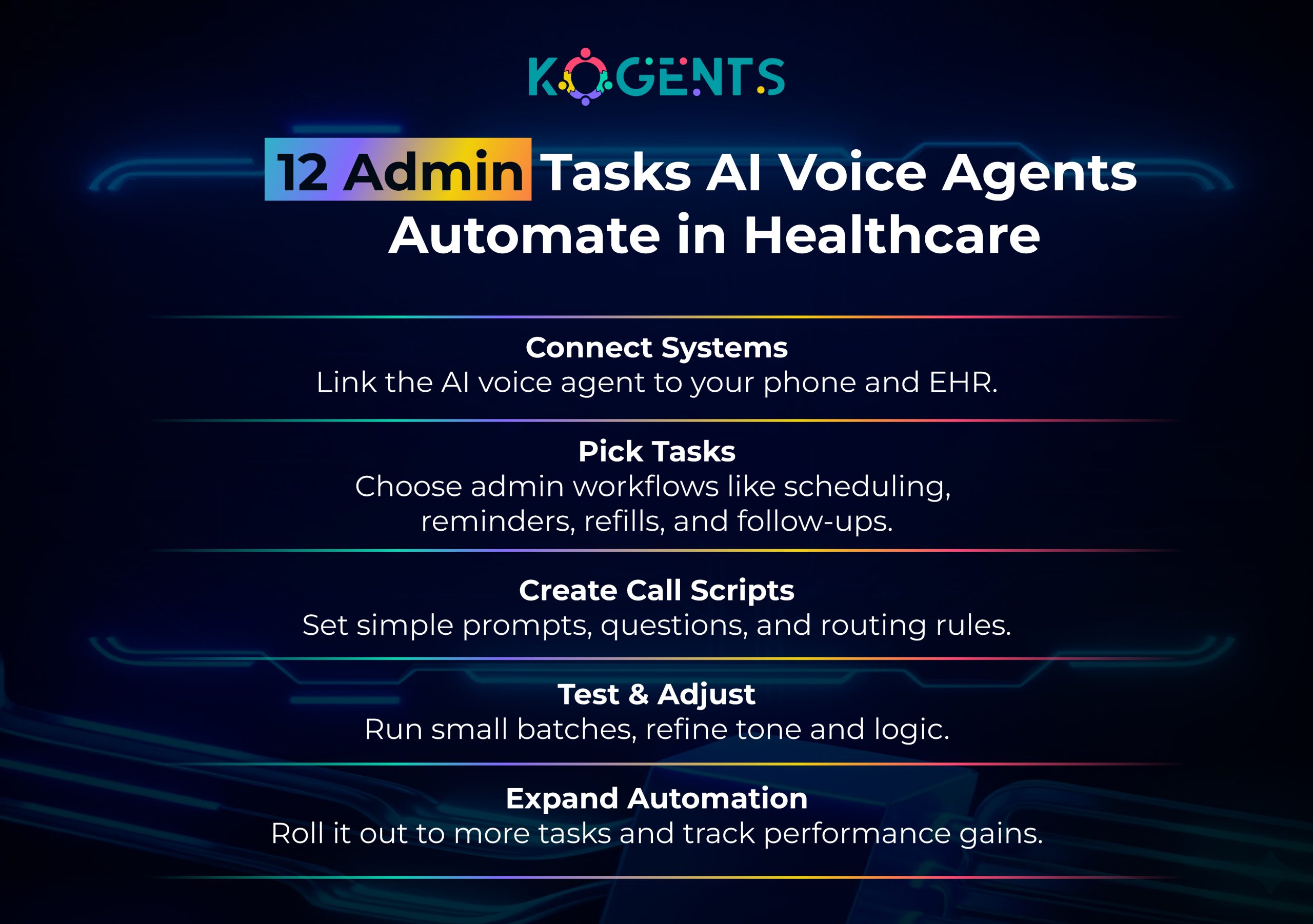
This is precisely where black bold AI voice agents for healthcare, autonomous, compliant, intelligent voicebots, create transformational value.
These black bold AI healthcare voice AI assistants, powered by speech recognition technology, natural language understanding (NLU), and automated medical workflows, can independently complete insurance verification calls, extract benefits data, synchronize results into EMR/EHR integration platforms, and eliminate human error at scale.
In this in-depth, you’ll learn how AI voice automation for health systems reverses revenue leakage and strengthens financial performance.
Key Takeaways
- Insurance verification and eligibility errors cause 25–35% of preventable claim denials, according to the U.S. Department of Health & Human Services (HHS).
- AI voicebots for hospitals complete payer calls 4–8× faster and provide higher documentation accuracy than manual staff.
- Organizations implementing black bold HIPAA-compliant AI voice agents recover $150,000 to over $1.2M annually by reducing verification gaps.
- AI medical voice AI systems operate 24/7, never fatigue, and eradicate administrative bottlenecks across insurance verification, prior authorization, and benefits checks.
- Voice-enabled healthcare automation creates scalable, predictable, and repeatable revenue cycle performance—no hold times, no human errors, no backlog.
The Growing Crisis of Revenue Leakage in Healthcare
Revenue leakage occurs whenever a provider delivers services but fails to receive proper reimbursement.
Among all leakage sources, insurance verification is the most prioritized avoidable cause, yet it remains one of the least optimized processes in healthcare.
Common Sources of Verification-Related Revenue Loss
- Incorrect or outdated insurance information
- Missing prior authorizations
- Failure to verify coverage before the visit
- Transcription/documentation mistakes
- Staff shortages are causing verification delays
- Appointment cancellations due to incomplete benefits data
- Incorrect copay/coinsurance entry
- Out-of-network surprises
This is precisely why organizations are migrating to black bold healthcare conversational AI voice tools, clinical agent AI voice assistant solutions, and medical practice voice automation software.
What Are AI Voice Agents for Healthcare?
Black bold AI voice agents for healthcare are fully autonomous, intelligent voicebots designed specifically for medical operations.
Unlike typical call center bots, these systems:
- Make outbound calls to insurance payers
- Navigate complex payer IVRs
- Ask eligibility questions
- Collect coverage details
- Extract structured data in real time
- Automatically log results in black bold EHR/EMR systems
- Follow compliant HIPAA standards
- Support multi-modal tasks (speech + data entry)
- Scale instantly without additional staffing
They combine:
- Black bold artificial intelligence (AI)
- black bold speech recognition
- black bold natural language processing (NLP)
- black bold call center automation
- black bold machine learning models
- black bold clinical decision support
- black bold ambient clinical intelligence
These capabilities allow them to fully automate insurance verification from start to finish.
Why Insurance Verification Is the Top Cause of Denials?
Insurance verification failures directly translate into:
- Denied claims
- Delayed reimbursements
- Lost patient revenue
- Increased A/R days
- Patient dissatisfaction
- Write-offs due to late prior auth
86% of denials are preventable, making proactive strategies a cornerstone of denial management.
The average cost to rework a denied claim ranges from $25 to $117.
Note: AI voice assistants for medical call centers solve these issues at scale.
How AI Voice Agents Streamline Insurance Verification Calls?
Let’s break down how AI phone agents for appointment scheduling, AI voice triage systems, and AI voice agents for patient intake automate the process.
1. Automatic Payer Calling (Outbound & Inbound)
AI agents:
- Dial insurers automatically
- Navigate IVRs with zero confusion
- Repeat calls until verification succeeds
- Never get fatigued by hold times
2. Intelligent IVR Navigation
The agent uses black bold natural language understanding (NLU) to interpret:
- Spoken prompts
- Numeric selections
- Multi-layer menus
3. Real-Time Eligibility & Benefits Extraction
AI collects:
- Active coverage status
- Plan details
- Deductible
- Copay
- Coinsurance
- Out-of-pocket max
- Prior authorization requirements
- Referral rules
4. Automated Documentation into EHR/EMR Systems
Through black bold EMR/EHR integration, data is:
- Logged automatically
- Structured as discrete fields
- Error-checked
- Ready for billing
5. Prior Authorization Detection
AI identifies services requiring authorization using:
- Historical rules
- Payer guidelines
- Procedure-specific data patterns
6. Zero Human Error
AI eliminates:
- Typos
- Misheard information
- Missed fields
- Inconsistent documentation
In short, AI delivers a fully automated medical workflow with near-perfect accuracy.
Why Healthcare Providers Are Shifting to AI Voice Automation?
1. 4–8× Faster Verification
AI handles calls in 2–4 minutes, compared to 30–45 minutes for staff.
2. Higher Accuracy
AI uses black bold speech-to-text, black bold clinical communication models, and black bold patient communication software to avoid errors.
3. 24/7 Availability
No staffing constraints. No missed verifications.
4. Significant Cost Savings
AI reduces verification cost per patient from:
- $7–$11 (manual) → <$1 (AI voice agent)
5. Better Compliance & Standardization
Supports:
- Black bold HIPAA compliance
- black bold HITRUST CSF
- black bold SOC 2 Type II
- black bold ISO/IEC 27001
6. Higher Patient Satisfaction
Accurate estimates reduce billing surprises.
Technology Deep-Dive: How AI Voice Agents Actually Work
To understand their power, let’s examine the core technologies behind black bold voice-enabled healthcare automation.
A. Natural Language Processing (NLP)
Interprets payer responses, coverage details, and spoken prompts.
B. Speech Recognition
Converts payer speech to text with 95–98% accuracy.
C. Machine Learning Models
Identify patterns, optimize routing, and detect missing data.
D. RPA for Healthcare
Automates:
- Data entry
- Field matching
- Documentation
- Chart updates
E. Ambient Clinical Intelligence
Allows AI to automatically structure payer data for clinical and financial teams.
F. Telehealth & Platform Integrations
Seamless with:
- Epic
- Cerner
- Athenahealth
- eClinicalWorks
- Allscripts
Case Studies: Real-World Impact of AI Voice Automation
Case Study 1: Multi-Specialty Clinic (Illinois)
Problem:
A 45-provider multi-specialty clinic was experiencing a 22% claim denial rate, primarily tied to missing insurance verification information and inconsistencies in benefits data entry. The front office team was overwhelmed, often rushing verification tasks or missing payer calls entirely due to high patient volume.
Solution:
The organization deployed black bold AI voicebots for hospitals to automate outbound verification calls, extract benefits information, identify prior authorization requirements, and sync results into their EHR.
Results:
- Denials dropped to 6%, driven by cleaner front-end data
- Verification turnaround reduced 87%, freeing up staff
- Annual recovered revenue: $420,000
Case Study 2: Radiology Network (Florida)
Problem:
A 17-location radiology network struggled with frequent prior authorization failures, resulting in patient delays, cancellations, and significant write-offs.
Staff reported spending up to 40 minutes per authorization, especially for MRI and CT claims with stringent payer requirements.
Solution:
The network implemented black bold medical voice AI platforms that performed automated payer outreach, confirmed authorization criteria, extracted procedure-level benefits, and flagged missing clinical notes needed for approval.
Results:
- 35% improvement in prior auth accuracy
- 62% reduction in preventable write-offs
- $780,000 annual savings
Case Study 3: Ambulatory Surgery Center (Texas)
Problem:
A busy ASC handling orthopedics and pain management was plagued by verification delays, leading to last-minute cancellations when insurance eligibility couldn’t be confirmed in time.
Their small front desk team was overwhelmed by payer call volumes, causing a backlog of 200+ pending verifications weekly.
Solution:
The ASC adopted black bold intelligent voice agents for medical practices to take over all insurance calls, verify coverage, extract surgical benefits, and document prior authorization requirements without human intervention.
Results:
- 50% reduction in staff workload
- 43% drop in claim denials
- 11× ROI in the first year
Outcome: The ASC gained the ability to confirm surgical benefits days earlier, leading to more accurate patient responsibility estimates and fewer surprise bills.
AI Voice Agents vs Human Staff
| Feature | Human Verification | AI Voice Agents |
| Time per verification | 30–45 mins | 2–4 mins |
| Accuracy | Medium | High (95–98%) |
| Labor cost | High | Very low |
| Hold time | Inevitable | Autonomous |
| Scalability | Limited | Unlimited |
| Compliance | Varies | Standardized |
| Availability | Business hours | 24/7 |
| Error risk | High | Zero fatigue |
Conclusion
Insurance verification is one of the most overlooked sources of financial loss in healthcare, but also one of the easiest to fix.
By leveraging black bold AI voice agents for healthcare, healthcare organizations can eliminate administrative bottlenecks, operate with greater financial predictability, reduce denials, and recover millions in lost revenue.
AI-driven automation is no longer optional; it is the new competitive advantage in modern healthcare operations.
If your organization wants to:
- Eliminate verification delays
- Reduce claim denials by 40–60%
- Automate payer calls 24/7
- Improve accuracy and compliance
- Reclaim revenue lost to administrative burden.
Our AI healthcare voice automation platform, Kogents.ai, delivers industry-leading speed, accuracy, and EHR-integrated scalability. So, what are you waiting for? Book a demo to see real ROI in action.
FAQs
How do AI voice agents for healthcare reduce revenue leakage?
By eliminating manual insurance verification delays and errors.
Are AI healthcare voice assistants HIPAA compliant?
Yes. They meet strict, black, bold HIPAA compliance guidelines.
Can AI voicebots for hospitals really replace staff?
They replace repetitive tasks, not staff—freeing humans for higher-level work.
How accurate are medical voice AI systems?
Most operate at 95–98% accuracy.
Do AI voice agents integrate with EHR/EMR platforms?
Yes—Epic, Cerner, Athenahealth, eCW, Allscripts, and more.
Can AI voice automation handle complex payer rules?
Yes—thanks to black bold machine learning models and black bold NLU.
Do AI voice agents work for small practices?
Absolutely—they scale up or down instantly.
How do they prevent claim denials?
By ensuring accurate eligibility, benefits, and prior authentication capture before the visit.
What’s the cost of implementing an AI voice automation system?
Usually, subscription-based SaaS pricing, far cheaper than manual verification.
Can AI voice agents assist with appointment scheduling?
Yes—through black bold AI phone agents for appointment scheduling**.
