Hospitals around the world are running beyond capacity. Nurse triage teams, already understaffed, face overwhelming surges during influenza seasons, RSV waves, heat crises, mass-casualty events, pandemics, and regional emergencies.
These failures don’t happen due to incompetence. They happen because human-only systems cannot scale during crisis-level surges.
This is where a healthcare AI assistant becomes a lifesaving operational layer.
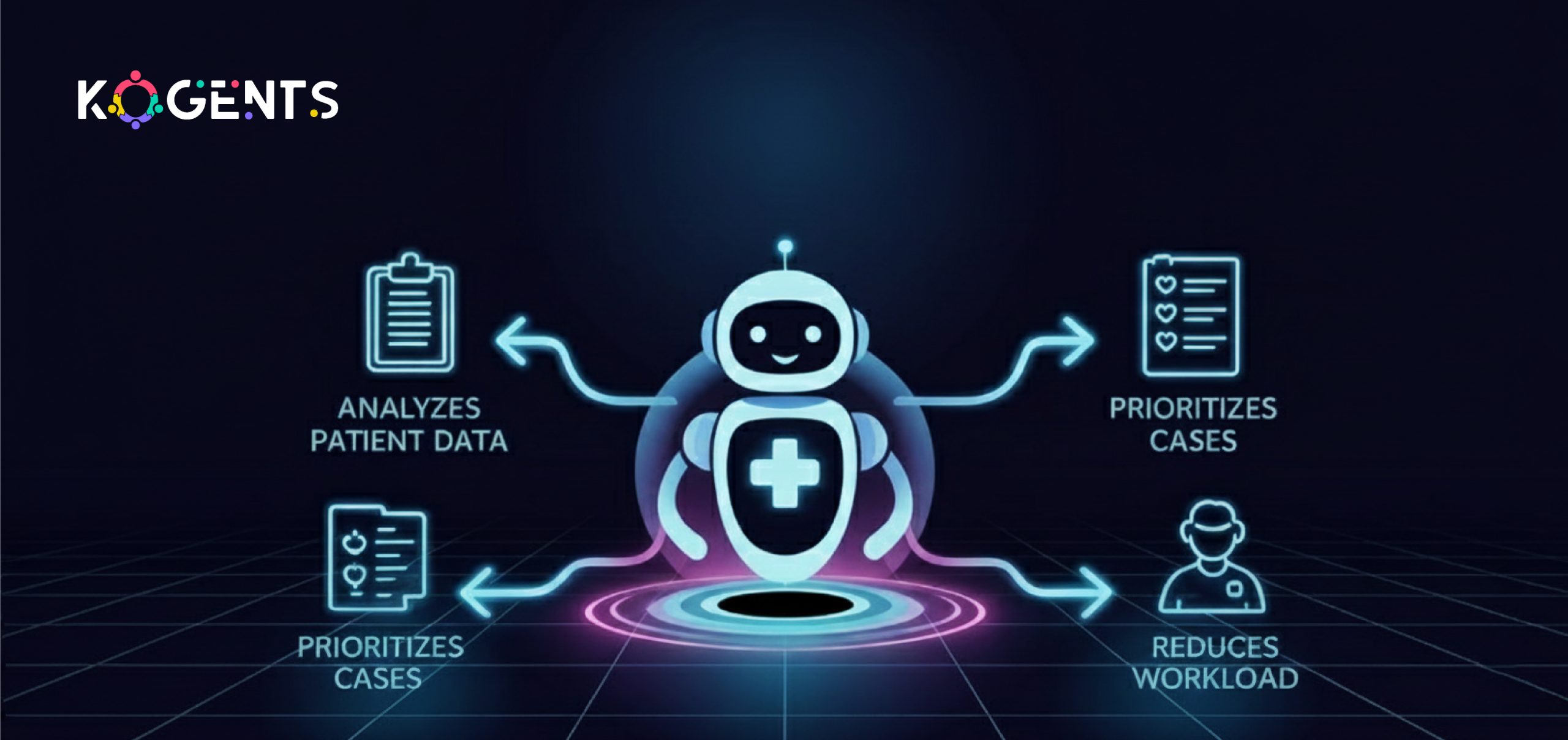
Instead of replacing nurses, it amplifies their capacity, automating what machines do best, freeing humans to focus on what only they can do.
Key Takeaways
- AI can reduce nurse triage handling time by 40–60%, based on McKinsey’s analysis of clinical workflow automation (McKinsey Healthcare AI Report).
- AI Agents for Healthcare Automation handles symptom intake, clinical documentation, patient messaging, risk scoring, and case routing, allowing nurses to focus on critical care.
- AI significantly improves surge resilience by absorbing thousands of low-acuity patient inquiries during crisis spikes.
- AI-driven decision support reduces clinical error rates, improves triage accuracy, and enhances patient safety with evidence-based guidance.
- AI increases operational capacity without requiring proportional increases in staffing, a crucial factor during public health emergencies.
Why Nurse Triage Teams Are Overwhelmed: The Modern Healthcare Strain?
Healthcare demand is outpacing supply in nearly every region. Key contributors include:
1. Increased Patient Volume
2. Workforce Shortages
3. Documentation Load
Nurses spend nearly 35% of their time on documentation alone, according to a study in JMIR Nursing.
4. Crisis Events Trigger Sudden Surges
Pandemics, heatwaves, wildfires, and mass casualty events can spike call volume 5–20× within hours.
5. Telehealth Growth
- Tele-triage calls rose 154% from 2019 to 2022, according to the CDC.
- Human teams cannot scale at crisis speed; AI can.
What Is a Healthcare AI Assistant?
A healthcare AI assistant is a secure, HIPAA-compliant digital assistant that supports clinicians by automating:
- Symptom collection
- Clinical documentation
- Patient communication
- Triage routing
- Decision support
- EHR/EMR charting
- Follow-up tasks
- Administrative workflows
It uses advanced technologies, natural language processing (NLP), machine learning, predictive analytics, clinical ontologies, and health informatics standards like HL7 FHIR.
Leading academic research from Nature Medicine and The Lancet Digital Health confirms that AI systems can now classify symptoms with human-level accuracy in many conditions.
How a Healthcare AI Assistant Supports Triage During Surges & Crisis Events?
Below is an expanded, research-backed breakdown of exactly how AI strengthens triage teams under extreme operational stress.
1. Advanced Symptom Intake & Pre-Triage Assessment
During surges, call volume can overwhelm triage nurses. A healthcare AI assistant acts as the first point of contact.
What it does:
- Collects patient symptoms through chat, voice, or phone
- Uses clinical protocols (e.g., Schmitt–Thompson triage guidelines)
- Runs evidence-based decision trees
- Identifies red-flag symptoms
- Summarizes findings for nurses
Evidence
This alone can reduce nurse workload by 30–50%.
2. AI-Driven Clinical Documentation Automation
One of the most significant bottlenecks in triage is documentation.
A clinical AI assistant can:
- Transcribe patient–nurse conversations
- Automatically prepare EMR-ready notes
- Tag ICD-10 codes
- Generate SOAP or HPI documentation
- Sync with Epic, Cerner (Oracle Health), Athenahealth, etc.
3. Intelligent Case Routing & Prioritization
During crises, minutes matter.
AI classifies cases into priority categories:
- High-acuity: chest pain, breathing issues, neuro deficits
- Moderate-acuity: uncontrolled symptoms
- Low-acuity: mild cold symptoms
- Self-care: guidance without escalation
Note: This eliminates queues filled with low-risk inquiries, ensuring critically ill patients receive attention.
4. Patient Communication Scaling During Crises
A virtual healthcare chatbot automates:
-
- Follow-up reminders
- Medication guidance
- Discharge instructions
- Symptom re-checks
- Telehealth prep
- Intake questionnaires
During surges, these tasks overwhelm staff; AI absorbs thousands at once.
Kaiser Permanente AI system clears 32% of patient messages.
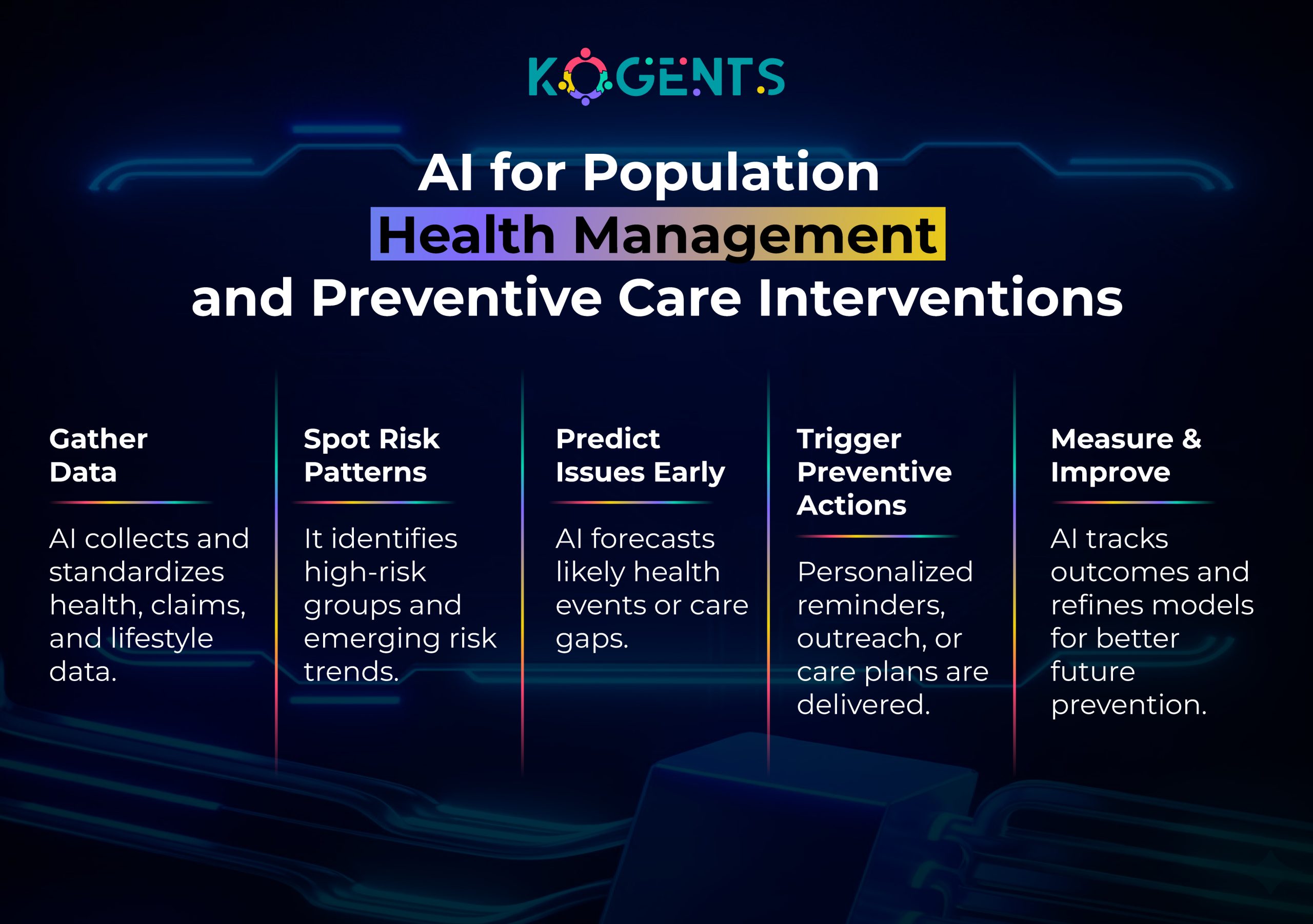
5. Predictive Analytics for Surge & Crisis Forecasting
Predictive AI models analyze:
- ED influx trends
- Local outbreak data
- Weather patterns
- Population health data
- Historical surge cycles
- Regional mobility patterns
According to a McKinsey analysis, predictive modeling reduces operational disruptions by up to 35%.
This allows leaders to pre-allocate staff and resources before the crisis peaks.
6. Telehealth & Remote Care Integration
A healthcare AI assistant bridges triage with virtual visits by:
- Pre-documenting symptoms
- Auto-scheduling telehealth appointments
- Preparing clinical notes for physicians
- Ensuring HIPAA-compliant routing
During crises, this moves a large percentage of care off-site.
7. Enhancing Clinical Safety with AI Decision Support
Agentic AI healthcare evidence-based guidance aligned with:
- CDC guidelines
- WHO clinical pathways
- American College of Emergency Physicians (ACEP)
- FDA SaMD AI/ML framework
This reduces decision variability during stressful high-volume periods.
8. Reducing Triage Abandonment Rates
- Without AI, patients may hang up after waiting too long.
- AI resolves many inquiries instantly, drastically reducing abandonment.
One Enhanced Table: AI Capabilities vs. Human Triage Capacity in Crisis Conditions
| Triage Function | Human-Only Workflow | With Healthcare AI Assistant | Capacity Increase |
| Symptom Intake | 10–15 minutes | 1–2 minutes automated | 85–90% faster |
| Documentation | 7–10 minutes | Auto-generated instantly | 100% saved |
| Call Handling | 12–20 minutes | 5–9 minutes | 50–60% faster |
| Follow-Ups | Manual | Automated at scale | 5× capacity |
| Routing | Manual prioritization | Instant AI classification | 10× precision |
| After-Hours Care | Nurse staffing limits | 24/7 AI support | Unlimited |
Regulatory, Security & Compliance Considerations
A healthcare AI agent must follow strict standards:
HIPAA
Protects patient privacy during data processing. HIPAA Summary – HHS
FDA SaMD (AI/ML) Guidelines
Ensures safety for clinical AI tools. FDA AI/ML SaMD
HL7 FHIR
For interoperability with EMRs. HL7 FHIR
ISO 27001 & SOC 2 Type II
- Security standards for healthcare SaaS systems.
- AI in healthcare must be auditable, explainable, transparent, and aligned with ethical best practices from sources like the World Economic Forum and AMA.
Case Studies
Case Study 1: Mayo Clinic – AI-Enhanced Symptom Triage During Pandemic Surges
During COVID-19, Mayo Clinic deployed AI-driven symptom assessors capable of handling thousands of simultaneous inquiries, helping the system stay operational during unprecedented call surges.
Case Study 2: Cleveland Clinic – AI Clinical Documentation to Offload Nurse Burden
Cleveland Clinic introduced AI-driven documentation using speech recognition and NLP.
It reduced note-taking time by 41%, enabling nurses to handle more triage calls and high-acuity cases.
Case Study 3: Kaiser Permanente – AI Chat Support for Flu Season Surges
Kaiser Permanente used a hybrid AI chatbot + nurse triage model that handled over 60% of low-acuity cases, allowing nurses to focus on severe care needs.
Case Study 4: Stanford Healthcare – AI-Based Predictive Modelling for ED Surges
Stanford Medicine deploys AI forecasting models predicting ED admission patterns up to 10 days in advance, drastically improving triage staffing readiness.
Future Trends: The Next Decade of AI-Augmented Nurse Triage
1. Agentic AI Workflows
AI that autonomously handles tasks:
- Auto-filling triage forms
- Ordering baseline labs (policy-permitting)
- Requesting vitals from remote monitors
2. Interoperable AI Across Care Continuums
Seamless transitions between ED, telehealth, urgent care, and clinics.
3. Digital Twins for Hospital Operations
AI creates real-time models of triage demand to optimize staffing.
4. Autonomous Documentation + Coding
Real-time ICD-10 coding and claims automation.
Before You Leave!
A healthcare AI assistant is not a futuristic tool; it is a present-day necessity for overwhelmed triage operations.
As patient volumes rise and crisis events become more frequent, healthcare systems must scale rapidly without compromising safety.
AI helps triage teams:
- Work faster
- Reduce cognitive load
- Improve patient safety
- Maintain care quality during surges
- Document efficiently
- Prioritize intelligently
Health systems that integrate AI now will be the ones best prepared for the next crisis.
If you want a HIPAA-compliant, clinically aligned, customizable healthcare AI assistant designed for triage automation, documentation support, and crisis scalability, explore Kogents.ai.
Visit us to request a demo and upgrade your triage capacity today.
FAQs
How does a healthcare AI assistant support nurse triage during surges?
It performs rapid symptom intake, prioritization, documentation, and routing, allowing nurses to focus on high-acuity patients.
Is a clinical AI assistant accurate enough for medical triage?
Academic studies (e.g., Lancet Digital Health) report accuracy up to 92% in triage assessments.
Can an AI healthcare assistant replace nurses?
No. It extends clinical capacity but does not make independent clinical decisions beyond preset protocols.
How does a virtual healthcare assistant protect patient data?
By following HIPAA, SOC 2 Type II, and ISO 27001 security frameworks.
Which hospitals currently use AI in triage?
Mayo Clinic, Cleveland Clinic, Kaiser Permanente, Stanford Medicine, and dozens more.
What tasks can an AI nurse assistant automate?
Documentation, follow-ups, symptom evaluation, routing, appointment scheduling, and more.
Does AI improve patient safety?
Yes, AI reduces triage variability by applying consistent, evidence-based decision logic.
How does AI integrate with telehealth?
It auto-documents symptoms, schedules virtual visits, and routes cases to providers.
Is a medical AI assistant cost-effective?
AI reduces overtime and improves throughput, often saving hospitals millions annually.
Can a healthcare AI assistant scale instantly during crises?
Yes, AI can handle thousands of triage interactions simultaneously without additional staffing.
